Cpt Code For Distal Soft Tissue Release
- Cpt Code For Distal Radius Fracture
- Cpt Code For Distal Soft Tissue Release
- Cpt Code For Distal Soft Tissue Release Date
CPT Code List
|
Number: 0629
CPT Code Defined Ctgy Description 24065 Biopsy, soft tissue of upper arm or elbow area; superficial 24066 Biopsy, soft tissue of upper arm or elbow area; deep (subfascial or intramuscular) 24071 Excision, tumor, soft tissue of upper arm or elbow area, subcutaneous; 3 cm or greater. August 2002 Bulletin. Bunionectomy codes. Procedures involve a distal soft tissue release (McBride), a resection of the base of the proximal phalanx (Keller),.
Policy
Simple Bunionectomy
(e.g., modified McBride, Silver Procedure)Aetna considers simple bunionectomy with soft tissue removal of the bump only without bony correction medically necessary in members with either of the following conditions:
- Members with clinical symptoms and a history of conservative management who meet the following criteria:
- Documentation of persistent pain and difficulty walking despite at least six months of conservative treatment under the direction of a healthcare professional which includes, but may not be limited to:
- Alternative or modified footwear
- Corticosteroid injections
- Debridement of hyperkeratotic lesions
- Foot orthotics (shoe inserts) (generally contractually excluded)
- Oral analgesics or nonsteroidal anti-inflammatory drugs (NSAIDS)
- Protective cushions/pads
- Radiographic confirmationFootnotes for Radiographic confirmation* of a hallux valgus angle (HVA) (formed by the long axis of the proximal phalanx and the first metatarsal) of 15 degrees or more with no degenerative changes at the meta-tarso-phalangeal (MTP) joint, and
- Documentation of skeletal maturity; or
- Documentation of persistent pain and difficulty walking despite at least six months of conservative treatment under the direction of a healthcare professional which includes, but may not be limited to:
- Members with diabetes who have an ulcer and/or infection stemming solely from the bunion.
Aetna considers simple bunionectomy experimental and investigational for all other indications because its effectiveness for indications other than the ones listed above has not been established.
Bony Correction Bunionectomy
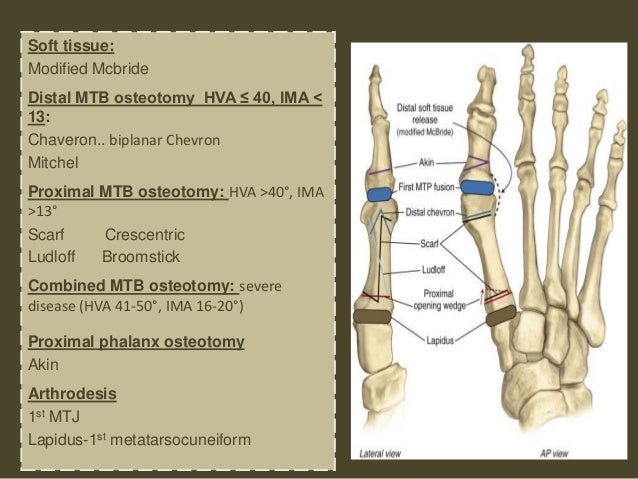
(e.g., Akin, Chevron, Keller, Lapidus, Mitchell, proximal metatarsal osteotomy procedures, etc.)Aetna considers bony correction bunionectomy medically necessary to treat symptomatic hallux valgus (bunion) in a skeletally mature individual (i.e., after epiphyseal closure) or an individual who is 18 years of age or older when the following criteria is met:
- The member's pain and symptoms over the medial bony eminence or calluses persist, making walking difficult despite at least a 6-month trial of conservative treatment under the direction of a healthcare professional that includes the following:
- Protective cushions/pads,
- Shoe inserts (generally contractually excluded),
- Corticosteroid injections,
- Debridement of hyperkeratotic lesions,
- Oral analgesics or non-steroidal antiinflammatory drugs (NSAIDs)
- Alternative or modified footwear that must include the following:
- Wearing well-fitting, low-heeled comfortable shoes made out of soft materials (e.g., canvas, cloth, soft leather) with wide toe box and padding; or
- Lace-ups or a combination last (front of the shoe is wider than the back of the shoe) that oconforms to the bunion and minimizes irritation; and
- Radiographic confirmationFootnotes for Radiographic confirmation* of the most recent weight-bearing view X-ray demonstrating both of the following:
- An HVA of 30 degrees or greater; and
- An inter-metatarsal angle (IMA) (formed by the long axis of the first and second metatarsals) of 12 degrees or greater; and
- Documentation of skeletal maturity; and
- The member has one or more of the following:
- A neuroma secondary to the bunion
- Problems with a dorsiflexed second toe due to over-riding of the great toe (so-called cross-over toe deformity)
- Limited or painful range of motion at the first toe MTP joint
- Painful prominence of the dorsiflexed second toe due to pressure from the first toe
- Ulceration caused by bunion
- Recurrent bursitis
- Demonstration of osteoarthritis on X-ray, as evidenced by any of the following:
- Cysts in the metatarsal head; or
- Loss of the cartilage space between the bones; or
- Mild-to-moderate bony proliferative pathology.
- The need for relief of a predisposing factor, e.g., Achilles tendon contracture.
Aetna considers bony correction bunionectomy experimental and investigational for all other indications because its effectiveness for indications other than the ones listed above has not been established.
Footnotes for Radiographic confirmation * Radiographic confirmation must include interpretation and report of weight bearing anterior/ posterior and lateral views of the affected foot.
Note: A bilateral bunionectomy done at the same time generally is not deemed medically necessary unless extenuating circumstances are present.
Aetna considers bony correction bunionectomy not medically necessary for the following indications:
- Foot ulcer(s) secondary to peripheral vascular disease; or
- Gangrene of the foot, ankle or lower leg; or
- Non-ambulatory individuals unless being performed to relieve ulceration due to prominence; or
- Open blisters, pressure sores, and skin ulceration overlying the bunion when the bunion is not the cause of the skin lesion (bony correction may lead to osteomyelitis); or
- Poor tissues at the operative site due to excessive scarring and multiple closely placed previous incisions; or
- Severe vascular insufficiency significantly impairing circulation to the foot (e.g., absent foot pulses, intermittent claudication, ankle/arm ratio less than 0.6); or
- To improve the appearance of the foot (cosmetic).
Surgical Correction of First Metatarsophalangeal (MTP) Joint
Aetna considers surgical correction of the first MTP joint (e.g., hallux rigidus) (including but not limited to arthrodesis (fusion), cheilectomy or the Keller procedure (resection arthroplasty)) medically necessary when the following criteria are met:
- Radiographic Footnotes for Radiographic confirmation*confirmation of osteoarthritis as evidenced by any of the following:
- Cysts in the metatarsal head; or
- Loss of the cartilage space between the bones; or
- Mild to moderate bony proliferative pathology; and
- Documentation of persistent pain and difficulty walking despite at least six months of conservative treatment under the direction of a healthcare professional which includes, but may not be limited to:
- Alternative or modified footwear
- Corticosteroid injections
- Debridement of hyperkeratotic lesions
- Foot orthotics (shoe inserts)(generally contractually excluded)
- Oral analgesics or nonsteroidal anti-inflammatory drugs (NSAIDS)
- Orthotics (shoe inserts) (generally contractually excluded)
- Protective cushions/pads; and
- Documentation of skeletal maturity.
Bunionette
Aetna considers correction of a bunionette deformity (tailor's bunion) (e,g., osteotomy or resection procedures) medically necessary in individuals with both of the following conditions:
- Radiographic confirmationFootnotes for Radiographic confirmation* of an IMA of 10 degrees or greater and the MTP angle is 16 degrees or greater; and
- Documentation of persistent pain and difficulty walking despite at least six months conservative treatment under the direction of a healthcare professional, which includes, but may not be limited to:
- Alternative or modified footwear (shoe modifications to ones that fit comfortably with a soft upper and a roomy toe box)
- Corticosteroid injections
- Debridement of hyperkeratotic lesions
- Foot orthotics (shoe inserts)(generally contractually excluded)
- Oral analgesics or nonsteroidal anti-inflammatory drugs (NSAIDS)
- Protective cushions/pads; and
- Documentation of skeletal maturity.
Aetna considers surgical correction of a bunionette deformity experimental and investigational for all other indications because its effectiveness for indications other than the ones listed above has not been established.
Cheilectomy
Aetna considers foot cheilectomy medically necessary for symptomatic relief of either of the following conditions:
- Painful bony spurs in the earlier stages of an arthritic joint; or
- Painful hallux rigidus meeting criteria for surgical correction of MTP joint noted above.
Cpt Code For Distal Radius Fracture
Aetna considers foot cheilectomy experimental and investigational for all other indications because its effectiveness for indications other than the ones listed above has not been established.
Arthrodesis
Aetna considers arthrodesis (fusion) of the foot medically necessary for any of the following conditions:
- A hallux valgus deformity when the second toe is absent; or
- Advanced hallux valgus (IMA greater than 20 degrees, HVA greater than 40 degrees); or
- Failed bony correction bunionectomy (e.g., Keller bunionectomy); or
- Failed cheilectomy; or
- Painful symptoms secondary to hallux valgus with advanced degenerative joint disease; or
- Painful symptoms secondary to hallux rigidus with advanced degenerative joint disease meeting criteria for MTP joint noted above: or
- Severely subluxated or dislocated MTP joints.
Aetna considers arthrodesis of the foot experimental and investigational for all other indications because its effectiveness for indications other than the ones listed above has not been established.
Allograft
Aetna considers the use of allograft in bunion repair experimental and investigational because its effectiveness for this indication has not been established.
Hits: 57 Van Morrison - Moondance Label: Warner Bros. Van morrison moondance reissue torrent.
Continuous Wound Infiltration with Local Anesthetics After Hallux Valgus Surgery
Aetna considers continuous wound infiltration with local anesthetics after hallux valgus surgery experimental and investigational because the effectiveness of this approach has not been established. See CPB 607 -- Anesthetic and Antiemetic Infusion Pumps.
See also
- CPB 0636 - Hammertoe Repair and
- CPB 0708 - Metatarsal Phalangeal Joint Replacement.
Background
Hallux valgus (bunion) is a common affliction of the adult foot caused by long-term irritation from poorly fitting shoes, arthritis, or heredity. The deformity usually develops after the age of 35 years and is often bilateral. It consists of a lateral deviation of the great toe, outward angulation of the metatarsal toward the other foot, separation of the heads of the first and second metatarsals, and prominent soft-tissue thickening over the medial surface of the head of the first metatarsal, commonly referred to as a bunion. Valgus posture of the great toe frequently causes a hammer toe-like deformity of the second toe. In addition, the splaying of the forefoot makes the wearing of shoes more difficult. With shoes that have a narrow toe box, corns often develop, as does bursal hypertrophy over the bunion. With the presence of valgus subluxation of the first meta-tarso-phalangeal (MTP) joint for a prolonged time, osteoarthritis frequently develops.
The tissues surrounding the joint may become inflamed and painful. However, not all bunion deformities may cause symptoms. A bunion has many etiologies including, but not limited to arthritic conditions, heredity or trauma, and the deformity is aggravated by faulty foot mechanics or tight fitting shoe wear. This progressive deformity is not a single disorder but complex deformity of the first ray or the column of bones that form the medial border of the fore foot.
Most bunions are treatable without surgery. Prevention is always best by choosing shoes that conform to the shape of the feet, have wide insteps, broad toes and soft soles. Patients should avoid shoes that are short, tight, sharply pointed, or with heels higher than 2¼ inches. If a bunion is already present, the patient should try protective pads to cushion the painful bunion and must wear well-fitting, low-heeled comfortable shoes that are roomy enough to not put pressure on it.
Surgery may be recommended to correct the deformity and reconstruct the bones and joints, restoring normal pain-free function to individuals having difficulty walking and/or experiencing pain despite accepted conservative treatments. Surgical repair of hallux valgus may include an osteotomy (cutting portions of bone on each side of the toe joint followed by realignment), shortening or lengthening tendons or ligaments, shaving tissue from the bunion, or arthrodesis (removing damaged portions of the joint and using screws, wires or a plate to hold the joint together). Several operative procedures and osteotomies have been devised and modified over time. The precise intervention employed depends on careful clinical and radiological evaluation and planning, as all hallux valgus deformities are unique and no single osteotomy procedure can treat them all.
Hallux valgus (lateral deviation of the great toe) is not a single disorder, as the name implies, but a complex deformity of the first ray that frequently is accompanied by deformity and symptoms in the lesser toes. Often, the intermetatarsal angle (IMA) formed by the long axis of the first and second metatarsals is more than the 8 to 9 degrees, which is usually considered to be the upper limits of normal. The hallux valgus angle (HVA), which measures the relationship of the long axis of the proximal phalanx and the first metatarsal, also is more than the 15 to 20 degrees, which is considered to be the upper limits of normal. If the hallux valgus angle of the first MTP joint exceeds 30 to 35 degrees, pronation of the great toe usually results.
In 2002, the Cochrane Library published its review on bunionectomy stating that an HVA of greater than 15 degrees is considered abnormal since at this angle the phalanx is no longer congruent with the metatarsal head. The joint may not become symptomatic until larger angles are reached or when the formation of a bunion begins, which is when the metatarsal head becomes very prominent and swelling develops medially over the joint.
According to the textbook Campbell's Operative Orthopaedics, bunion deformities are divided into 3 stages:
| Stage | Characteristics | IMA | HVA |
|---|---|---|---|
| Mild |
| < 12° | 21 - 30° |
| Moderate |
| 12 -16° | 31 - 40° |
| Severe |
| > 16° | > 40° |
Under accepted guidelines, surgery is recommended to correct the deformity, reconstruct the bones and joint, and restore normal, pain-free function when the bunion has progressed to a level where the patient has difficulty walking and/or experiences pain despite accommodative shoes and presents itself with angular deformities corresponding to a moderate to severe stage (see above). In addition, the presentation of a number of complications directly related to bunion formation may cause need for either soft tissue correction of the hallux valgus complex and/or concomitant bony correction. Inadequate vascularity or sensibility should be investigated thoroughly before any bunion surgery is considered.
There are many different surgical procedures available for treatment of hallux valgus, ranging from the very simple to the highly technical. They have endured the clinical test of adequate numbers of patients, lengthy and detailed review, and reports by multiple observers using essentially the same techniques.
The usual candidate for the Silver Procedure, a simple exostectomy with removal of the bunion only, is a 30- to 50-year old woman with clinical symptoms from a prominent bunion, an IMA of less than 12 degrees, an HVA of 15 to 25 degrees with no degenerative changes at the MTP joint, and a history of conservative management failure. Typically, this procedure is performed along with other hallux valgus reconstructive procedures such as Chevron, McBride, or proximal osteotomy.
In properly selected patients with stress (weight-bearing) view roentgenograms showing the medial capsule acting as a spring on stretch of the MTP joint, the modified McBride bunionectomy may be indicated. It involves removal of the bunion as well as rebalancing of the big toe joint by releasing the tight tendons on the lateral side (side nearest to the 2nd toe) and tightening the joint capsule on the medial side and sometimes removing one of the sesamoid bones. This procedure is utilized when there is a positional hallux valgus, i.e., the big toe is drifted over toward the 2nd toe but there are no significant bones or structural deformities other than the bunion bump.
Candidates for the Keller procedure, combined soft tissue release and removal of the medial eminence with resection of the proximal end of the proximal phalanx, are patients between 55 and 70 years of age with moderate-to-severe hallux valgus (30 to 45 degrees) and/or significant joint arthrosis (hallux limitus or rigidus), IMAs of 12 degrees or less, and pain over the medial or dorsal eminence with any shoe worn so that the variety of shoes the patient can wear is severely limited. An incongruous first MTP joint caused by lateral subluxation of the phalanx on the metatarsal head, severe lateral displacement of the sesamoids, and any evidence of degenerative cartilage changes in the joint are all roentgenographic indications for the Keller procedure.
The Akin procedure is used for correction of hallux valgus interphalangeus when the deformity is located at the interphalangeal joint. In this procedure, a medially based closing-wedge osteotomy of the proximal phalanx is performed, the medial eminence of the first metatarsal head is resected, and medial capsular reefing is done. Usually the Aiken is performed along with a Silver or McBride procedure.
First metatarsal head osteotomies are probably the most commonly performed bunionectomy procedures today. The choice of osteotomy performed is dependent upon both the perceived etiology of the condition and the amount of correction required. In younger patients with no joint arthrosis, and with mild-to-moderate hallux valgus deformities (IMA angle less than 16 and HVA less than 30 to 35 degrees), a Chevron (Austin) osteotomy may be the procedure of choice. It involves a 'V' shaped osteotomy of the distal metatarsal, which allows the first metatarsal head to be shifted laterally, correcting the abnormal shape from long standing valgus drift. According to the literature, a proximal metatarsal osteotomy for hallux valgus is indicated for patients with moderate-to-severe deformities (HVA of 13 to 20 degrees), and may be combined with other hallux valgus reconstructive procedures such as resection of medial eminence (Silver procedure) or a McBride type of soft tissue release.
The literature indicates that the Mitchell bunionectomy is applicable to moderate to severe deformities of the intermetatarsal angle and hallux valgus and consists of a metatarsal osteotomy that displaces metatarsal head laterally in order to correct hallux valgus deformity and metatarsus adductus. This procedure is carried out more proximally than the Chevron osteotomy and can correct more severe deformities than Chevron.
Lee et al (2008) noted that proximal Chevron osteotomy (PCO) for hallux valgus is inherently more stable than the other forms of proximal metatarsal osteotomy, but complications, such as, delayed union, nonunion, and malunion can occur. These researchers compared results of two axial Kirschner wire fixation with or without transverse Kirschner wires in PCO for moderate-to-severe hallux valgus deformities. A prospective study was conducted on 65 patients (85 feet) who underwent PCO and a distal soft tissue procedure for moderate-to-severe hallux valgus. Patients were divided into 2 groups- 2 axial Kirschner wire fixation (group I) ,and
- 2 axial and supplementary transverse Kirschner wire fixation (group II).
- simultaneous bilateral surgical group (group A), and
- an unilateral surgical group (group B).
Bunionette or tailor’s bunion is a bony prominence on the lateral side of the metatarsal head or the fifth toe. A bunionette is often combined with a bunion or hallux valgus known as 'splay foot' or is seen congenitally or may be enlarged due to trauma. A painful callus or a localized keratosis may form beneath the fifth metatarsal head along with the bursa on the lateral side of the toe. Surgical repair may be necessary when severe pain limits an individual’s ability to walk.
Like a bunion, a bunionette deformity (tailor's bunion, overlapping or underlapping 5th toe deformity) may be created by a wide intermetatarsal angle between the 4th and 5th metatarsals. The normal 4th and 5th IMA is approximately 6.2 degrees, and the normal 5th MTP angle is about 10 degrees. Pathological angles are in the range of 10 degrees for the IMA and 16 degrees for the MTP angle. Pressure placed on the head of the 5th metatarsal exacerbated by tight shoes forms a painful osseous prominence, hypertrophy, and/or signs of inflammation on the outside of the foot near the base of the little toe. It may be associated with a symptomatic plantar callus, a hard corn and painful bursitis. According to accepted guidelines, treatment should initially consist of conservative measures; this includes padding, debridement, NSAIDS, orthotic therapy, and shoe modifications to ones that fit comfortably with a soft upper and a roomy toe box. In cases where non-operative treatment can no longer control the symptoms of persistent pain, surgical intervention is warranted. Soft tissue surgery does not solve the problem as the offending agent is usually the head of the 5th metatarsal. A proximal osteotomy is able to correct most deformities. The literature indicates a distal osteotomy is recommended if medial translation of the head for 1/3 of the width of the metatarsal shaft produces a normal 4th to 5th IMA. A partial ostectomy of the 5th metatarsal may be adequate if IMA reduction is not indicated.
Degenerative joint disease may develop over the years and includes erosion of cartilage, joint space narrowing and varying amounts of bony spurs around the 1st MTP joint. Milder cases may consist of slight limitation of motion and little pain. More severe cases may consist of a rigid joint and considerable pain. Cheilectomy is a procedure that may be utilized in earlier stages of an arthritic joint in which there are painful bone spurs. The bony irregularities are shaved off and the cartilage may also be remodeled.
The great toe is stabilized in part by the presence of 2nd toe and, when it is absent, a hallux valgus deformity is best treated by arthrodesis of first MTP joint. Another indication for arthrodesis includes a failed Keller bunionectomy. Fusion is the procedure of choice for hallux valgus associated with advanced degenerative joint disease, and advanced hallux valgus (IMA greater than 20 degrees, HVA greater than 40 degrees), severely subluxated or dislocated MTP joints, or for failed hallux valgus surgery. Cheilectomy is not the procedure of choice in presence of advanced degenerative joint changes. The Lapidus procedure is indicated for patients with severe hallux valgus deformity accompanied by a hypermobile 1st ray. The procedure involves arthrodesis of the metatarsalcuneiform joint.
Hallux rigidus is a progressive disorder characterized by limitation of movement along with a dorsal bunion at the MTP joint of the great toe most often caused in an adult by degenerative arthritis. An individual with hallux rigidus may have history of pain and stiffness in the first MTP joint increased with activity and aggravated by shoes. Many surgical procedures for hallux rigidus have been recommended including but not limited to arthrodesis (fusion), cheilectomy or the Keller procedure (resection arthroplasty).
Hallux limitus and hallux rigidus is, as their names imply, a loss of flexibility of the great toe as a result of osteoarthritic or degenerative changes at the first MTP joint. This may be more disabling than hallux valgus, because the patient is unable to achieve relief even when not wearing shoes. It is usually unilateral and is distinguished from hallux valgus by the lack of angular deformity (the alignment remaining normal) and by the prominence of the osteoarthritic changes at the dorsal surface of the joint, asymmetrical joint-space narrowing, subchondral sclerosis, marginal spurs, and, at times, rather large subchondral cysts. Cheilectomy, which includes not only excision of the dorsal bone spur but also the dorsal third of the metatarsal head, gives long-term pain relief in most patients. Cheilectomy involves removal of the proliferative bone from the metatarsal head so as to remove the buttress preventing dorsiflexion of the proximal phalanx on the metatarsal head. Arthrodesis or a Keller procedure is the generally accepted treatment of choice following failed cheilectomy or where advanced degenerative changes are present.
In a case-series study, Masquijo et al (2010) evaluated the results of a 5th metatarsal sliding osteotomy for the treatment of this deformity in patients under 18 years of age. These researchers retrospectively evaluated 13 feet in 11 consecutive patients with bunionette deformity treated from January 2003 to January 2008 at 2 referral centers. Mean age was 14.8 years (95 % confidence limit, SD 1.5 years); mean follow-up was 32.2 months (95 % confidence limit, SD 11.7 months); and clinical evaluation was made according to the modified AOFAS score and the Coughlin score. The IV-V IMA ( IV-V IMA), the width of the forefoot (WF), lateral deviation angle (LDA), and 5th metatarsophalangeal angle (5 MPA) were also measured pre-operatively and post-operatively. The average post-operative AOFAS score was 91 +/- 4.1 points. Seven patients (8 feet) had an excellent outcome and 4 patients (5 feet) a good outcome according to the Coughlin scoring rate. The IV-V IMA averaged 12.29 degrees +/- 1.5 degrees pre-operatively, while post-operatively it was 6.18 degrees +/- 1.4 degrees (p < 0.0001). The LDA improved from 7.74 degrees +/- 1.7 degrees pre-operatively to 4.25 degrees +/- 1 degree after surgery (p < 0.0001). The WF decreased from 8.01 +/- 1.3 mm to 7.05 +/- 1.3 mm (p < 0.0001). The mean 5 MPA decreased from 21.7 degrees +/- 4.1 degrees pre-operatively to 7.63 degrees +/- 3.4 degrees at final follow-up (p < 0.0001). One patient developed a superficial infection around a K-wire. The authors concluded that metatarsal sliding osteotomy is a safe and effective method for the correction of symptomatic bunionette in patients below 18 years of age. Moreover, they stated that further research is needed to compare this approach with other treatment methods in this specific age group.
Guha et al (2012) noted that the bunionette or tailor's bunion is a lateral prominence of the 5fth metatarsal head. It is usually characterized by a wide IMA between the 4th and 5th metatarsals, varus of the MTP joint, pain and callus formation. Various distal, shaft and basal osteotomies have been described in the literature. These investigators have described a reverse scarf osteotomy for bunionette correction. They have used a 'reverse' scarf osteotomy in 12 cases (10 females: 2 males) with a mean follow-up of 12 months (range of 5 to 22 months) with radiographs and clinical scoring. Post-operatively, mean IMA improved from 13.1 degrees to 7.27 degrees (range of 2.0 to 11.5); mean 5th MTP angle improved from 19.9 degrees to 6.36 degrees (range of 2.8 to 9.0) and post-operative mean AOFAS improved from 54.25 to 89.58 (range of 70 to 100). The authors concluded that 'reverse' scarf osteotomy in the correction of bunionette deformity offers promising results in the short-term.
An UpToDate review on “Hallux valgus deformity (bunion)” (Ferrari, 2013) does not mention the use of allograft as a therapeutic option.
Chao and colleagues (2013) stated that the standard treatment for hallux valgus in rheumatoid arthritis (RA) has been arthrodesis of the first MTP joint. There is limited literature regarding the results of hallux valgus procedures which preserve the first MTP joint in RA. These researchers investigated the radiographic and clinical outcomes of joint-preserving surgery for hallux valgus in a series of RA patients to evaluate the result of non-arthrodesis reconstruction. A total of 37 feet with hallux valgus in 27 patients with RA treated with a joint-preserving procedure of the first MTP joint were analyzed radiographically and clinically. Average follow-up was 42 (range of 12 to 111) months; 20 feet had Ludloff osteotomies, 15 had scarf osteotomies, and 2 had chevron osteotomies. Radiographs were evaluated pre-operatively and post-operatively for hallux valgus angle, 1-2 intermetatarsal angle, and degenerative narrowing of the first MTP joint based the Sharp score and the Larsen grade. Narrowing of the first inter-phalangeal (IP) joint was based on a modification of the classification of Hattrup and Johnson. Operative complications and required secondary surgeries were tabulated. Clinical outcomes were measured using pre-operative and post-operative Short Form-36 (SF-36), AOFAS forefoot scale, and visual analog scale (VAS) pain questionnaires. The average hallux valgus angle improved from 37 degrees pre-operatively to 15 degrees post-operatively. The average 1-2 intermetatarsal angle improved from 14 degrees pre-operatively to 5 degrees post-operatively. The average Sharp score of the first MTP joint was 0.9 pre-operatively and 1.6 post-operatively. The average Larsen grade of the first MTP joint was 0.6 pre-operatively and 1.4 post-operatively. Range of motion of the first MTP joint was essentially unchanged between pre-operative and post-operative measurements. Seven of 37 feet had progression of first IP joint space narrowing, but none was symptomatic. The AOFAS score improved from 45.2 pre-operatively to 82.6 at final follow-up (p < 0.01). The VAS decreased from 4.8 pre-operatively to 1.5 at final follow-up (p < 0.02). The SF-36 physical component score decreased from 40.3 pre-operatively to 37.4 at final follow-up, and the mental component score remained unchanged, and neither was statistically significant. There were 7 feet (19 %) that required a return to surgery: 3 wound infections, 2 arthrodeses for progression of deformity, and 1 each for revision for recurrence and hardware removal. The authors concluded that RA patients who undergo a bunionectomy rather than arthrodesis to preserve the first MTP joint have satisfactory clinical and radiographic outcomes. This procedure appeared to be a reasonable alternative to first MTP arthrodesis in patients with relatively preserved joints.
Cheilectomy Versus Decompression Osteotomy in Early-Stage Hallux Rigidus
Cullen and colleagues (2017) noted that 2 commonly used procedures for early stage hallux rigidus are- cheilectomy and
- decompression metatarsal osteotomy.
However, although both procedures were first described several decades ago, a deficit exists in the published data comparing their effectiveness. These investigators performed a retrospective comparative study to examine the results of surgical treatment of early-stage hallux rigidus. A total of 423 subjects were included in this study. Hallux limitus or rigidus had been diagnosed in all patients, who had undergone either cheilectomy or any variation of plantar-flexion decompression metatarsal head osteotomy. Of the 423 procedures identified during the study period, 341 (80.6 %) were cheilectomy and 82 (19.4 %) were decompression osteotomy procedures. The rate of revision procedures was significantly greater in the cheilectomy group (8.21 %) than in the osteotomy group (1.22 %). Sex, laterality, and body mass index (BMI) played no role in the rate of revision. The absence of research studies comparing the effectiveness of the 2 procedures has led many practitioners to favor cheilectomy for early-stage hallux rigidus. Decompression metatarsal osteotomies are technically more difficult, involve more risks, and require greater restrictions on postoperative weight-bearing compared with cheilectomy. The authors concluded that these findings demonstrated that within the first 5 post-operative years, decompression osteotomy resulted in a dramatically lower rate of revisional surgery for 1st MTP joint pathology compared with cheilectomy.
Cpt Code For Distal Soft Tissue Release
Continuous Wound Infiltration with Local Anesthetics After Hallux Valgus Surgery
Braito and colleagues (2018) noted that hallux valgus surgery is associated with significant early post-operative pain. In a prospective, randomized, double-blind, and placebo-controlled, single-center trial, these investigators examined the use of continuous wound infiltration (CWI) with ropivacaine for pain management after hallux valgus surgery. A total of 50 patients undergoing distal metatarsal osteotomy for idiopathic hallux valgus were allocated to CWI with ropivacaine 2 mg/ml at a rate of 2 ml/hr or placebo for 24 hours post-operatively. Average and peak pain levels on the verbal numeric rating scale (NRS; 1 to 10) during the 1st 48 hours after surgery were recorded as primary outcome parameters. Secondary outcome parameters included consumption of narcotics, clinical outcome, incidence of post-operative complications, and patient satisfaction. No significant difference in mean (p = 0.596) and peak (p = 0.353) post-operative pain level was found for CWI with either ropivacaine (mean NRS 1.9 ± 0.8; peak NRS 3.5 ± 2.0) or placebo (mean NRS 2.0 ± 0.7; peak NRS 3.9 ± 1.7) during the early post-operative course. Furthermore, no significant differences between both groups were detected regarding narcotic consumption (p = 0.354) and all other secondary outcome parameters; 2 severe complications (local dysesthesia with CWI, catheter accidentally fixed by a suture) and 5 catheter dislocations were observed. The authors concluded that CWI with ropivacaine 2 mg/ml at a rate of 2 ml/hr for 24 hours after hallux valgus surgery did not reduce post-operative pain level in an in-patient setting. Level of Evidence = I.
Furthermore, an UpToDate review on “Hallux valgus deformity (bunion)” (Ferrari, 2018) does not mention continuous wound infiltration as a tool for post-operative management.
| Code | Code Description |
|---|---|
Information in the [brackets] below has been added for clarification purposes. Codes requiring a 7th character are represented by '+': | |
Simple bunionectomy: | |
CPT codes covered if selection criteria are met: | |
| 28290 | Correction, hallux valgus (bunion), with or without sesamoidectomy; simple exostectomy (e.g., Silver type procedure) |
CPT codes not covered for indications listed in the CPB (not all-inclusive): | |
Continuous wound infiltration with local anesthetics - no specific code: | |
Other CPT codes related to the CPB: | |
| 11055 - 11057 | Paring or cutting of benign hyperkeratotic lesion (eg, corn or callus) |
| 73620 | Radiologic examination, foot; 2 views |
| 73630 | Radiologic examination, foot; complete, minimum of 3 views |
Other HCPCS codes related to the CPB: | |
| J0702 | Injection, betamethasone acetate 3 mg and betamethasone sodium phosphate 3 mg |
| J1020 | Injection, methylprednisolone acetate, 20 mg |
| J1030 | Injection, methylprednisolone acetate, 40 mg |
| J1040 | Injection, methylprednisolone acetate, 80 mg |
| J1094 | Injection, dexamethasone acetate, 1 mg |
| J1100 | Injection, dexamethasone sodium phosphate, 1 mg |
| J1700 | Injection, hydrocortisone acetate, up to 25 mg |
| J1710 | Injection, hydrocortisone sodium phosphate, up to 50 mg |
| J1720 | Injection, hydrocortisone sodium succinate, up to 100 mg |
| J1741 | Injection, ibuprofen, 100 mg |
| J1885 | Injection, ketorolac tromethamine, per 15 mg |
| J2920 | Injection, methylprednisolone sodium succinate, up to 40 mg |
| J3300 | Injection, triamcinolone acetonide, preservative free, 1 mg |
| J3301 | Injection, triamcinolone acetonide, not otherwise specified, 10 mg |
| J3302 | Injection, triamcinolone diacetate, per 5 mg |
| J7312 | Injection, dexamethasone, intravitreal implant, 0.1 mg |
| L3000 - L3100 | Foot inserts and arch supports |
| L3201 - L3265 | Orthopedic footwear |
ICD-10 codes covered if selection criteria are met: | |
| E10.51 - E10.59 E11.51 - E11.59 E13.51 - E13.59 | Diabetes with circulatory complications [with ulcer and/or infection stemming solely from bunion] |
| L89.890 - L89.899 | Pressure ulcer of other site [toes] [in diabetic members stemming solely from bunion] |
| L97.501 - L97.529 | Non-pressure ulcer of other part of foot [toes] [in diabetic members stemming solely from bunion] |
| M20.10 - M20.12 | Hallux valgus (acquired) |
| M21.611 - M21.619 | Bunion |
| M86.071 - M86.079, M86.171 - M86.179 M86.271 - M86.279, M86.371 - M86.379 M86.471 - M86.479, M86.571 - M86.579 M86.9 | Osteomyelitis, periositis, and other infections involving bone [stemming solely from bunion] |
Bony Correction Bunionectomy (e.g., Akin, Chevron Osteotomy, Keller, Mitchell, proximal metatarsal osteotomy procedures, etc.): | |
Allograft for bunion repair - no specific code: | |
CPT codes covered if selection criteria are met: | |
| 28292 | Correction, hallux valgus (bunion), with or without sesamoidectomy; Keller, McBride or Mayo type procedure |
| 28294 | Correction, hallux valgus (bunion), with or without sesamoidectomy; with tendon transplants (e.g., Joplin type procedure) |
| 28295 | Correction, hallux valgus (bunionectomy), with sesamoidectomy, when performed; with proximal metatarsal osteotomy, any method |
| 28296 | Correction, hallux valgus (bunion), with or without sesamoidectomy; with metatarsal osteotomy (e.g., Mitchell, Chevron or concentric type procedures) |
| 28297 | Correction, hallux valgus (bunion), with or without sesamoidectomy; Lapidus type procedure |
| 28298 | Correction, hallux valgus (bunion), with or without sesamoidectomy; by phalanx osteotomy |
| 28299 | Correction, hallux valgus (bunion), with or without sesamoidectomy; by double osteotomy |
CPT codes not covered for indications listed in the CPB (not all-inclusive): | |
Continuous wound infiltration with local anesthetics - no specific code: | |
Other CPT codes related to the CPB: | |
| 11055 - 11057 | Paring or cutting of benign hyperkeratotic lesion (eg, corn or callus) |
| 73620 | Radiologic examination, foot; 2 views |
| 73630 | Radiologic examination, foot; complete, minimum of 3 views |
Other HCPCS codes related to the CPB: | |
| A5512 - A5513 | For diabetics only, multiple density inserts |
| J0702 | Injection, betamethasone acetate 3 mg and betamethasone sodium phosphate 3 mg |
| J1020 | Injection, methylprednisolone acetate, 20 mg |
| J1030 | Injection, methylprednisolone acetate, 40 mg |
| J1040 | Injection, methylprednisolone acetate, 80 mg |
| J1094 | Injection, dexamethasone acetate, 1 mg |
| J1100 | Injection, dexamethasone sodium phosphate, 1 mg |
| J1700 | Injection, hydrocortisone acetate, up to 25 mg |
| J1710 | Injection, hydrocortisone sodium phosphate, up to 50 mg |
| J1720 | Injection, hydrocortisone sodium succinate, up to 100 mg |
| J1741 | Injection, ibuprofen, 100 mg |
| J1885 | Injection, ketorolac tromethamine, per 15 mg |
| J2920 | Injection, methylprednisolone sodium succinate, up to 40 mg |
| J3300 | Injection, triamcinolone acetonide, preservative free, 1 mg |
| J3301 | Injection, triamcinolone acetonide, not otherwise specified, 10 mg |
| J3302 | Injection, triamcinolone diacetate, per 5 mg |
| J7312 | Injection, dexamethasone, intravitreal implant, 0.1 mg |
| L3000 - L3100 | Foot inserts and arch supports |
ICD-10 codes covered if selection criteria are met: | |
| D21.20 - D21.22 | Benign neoplasm of connective and other soft tissue of lower limb, including hip |
| G57.60 - G57.63 | Lesion of plantar nerve [neuroma secondary to bunion] |
| M19.071 - M19.079 | Primary osteoarthritis ankle and foot |
| M19.171 - M19.179 | Post-traumatic osteoarthritis, ankle and foot |
| M20.10 - M20.12 | Hallux valgus (acquired) |
| M20.5x1 - M20.5x9 | Other deformities of toe(s) (acquired) [overriding of great toe or crossover toe deformity] |
| M21.611 - M21.629 | Bunion |
| M67.00 - M67.02 | Short Achilles tendon (acquired) |
| M71.171 - M71.179 | Other infective bursitis, ankle and foot [recurrent] |
| M77.50 - M77.52 | Other enthesopathy of foot [recurrent bursitis] |
| M85.671 - M85.679 | Other cyst of bone, ankle and foot |
| Q66.89 | Other specified congenital deformities of feet [overriding of great toe or crossover toe deformity] |
ICD-10 codes not covered for indications listed in the CPB: | |
| I73.9 | Peripheral vascular disease, unspecified [severe vascular insufficiency impairing circulation] |
| I96 | Gangrene, not elsewhere classified [of the foot, ankle or lower leg] |
| L89.890 - L89.899 | Pressure ulcer of other site [toes] [Open blisters, pressure sores, and skin ulceration overlying the bunion when the bunion is not the cause of the skin lesion or secondary to peripheral vascular disease] |
| L97.501 - L97.529 | Non-pressure ulcer of other part of foot [toes] [Open blisters, pressure sores, and skin ulceration overlying the bunion when the bunion is not the cause of the skin lesion or secondary to peripheral vascular disease] |
| M24.671 - M24.676 | Ankylosis, ankle and foot [excessive scarring] |
| Z74.01 | Bed confinement status [non-ambulatory individuals] |
Bunionette: | |
CPT codes covered if selection criteria are met: | |
| 28110 | Ostectomy, partial excision, fifth metatarsal head (bunionette) (separate procedure) |
Other CPT codes related to the CPB: | |
| 11055 - 11057 | Paring or cutting of benign hyperkeratotic lesion (eg, corn or callus) |
| 73620 | Radiologic examination, foot; 2 views |
| 73630 | Radiologic examination, foot; complete, minimum of 3 views |
Other HCPCS codes related to the CPB: | |
| J0702 | Injection, betamethasone acetate 3 mg and betamethasone sodium phosphate 3 mg |
| J1020 | Injection, methylprednisolone acetate, 20 mg |
| J1030 | Injection, methylprednisolone acetate, 40 mg |
| J1040 | Injection, methylprednisolone acetate, 80 mg |
| J1094 | Injection, dexamethasone acetate, 1 mg |
| J1100 | Injection, dexamethasone sodium phosphate, 1 mg |
| J1700 | Injection, hydrocortisone acetate, up to 25 mg |
| J1710 | Injection, hydrocortisone sodium phosphate, up to 50 mg |
| J1720 | Injection, hydrocortisone sodium succinate, up to 100 mg |
| J1741 | Injection, ibuprofen, 100 mg |
| J1885 | Injection, ketorolac tromethamine, per 15 mg |
| J2920 | Injection, methylprednisolone sodium succinate, up to 40 mg |
| J3300 | Injection, triamcinolone acetonide, preservative free, 1 mg |
| J3301 | Injection, triamcinolone acetonide, not otherwise specified, 10 mg |
| J3302 | Injection, triamcinolone diacetate, per 5 mg |
| J7312 | Injection, dexamethasone, intravitreal implant, 0.1 mg |
| L3000 - L3100 | Foot inserts and arch supports |
| L3201 - L3265 | Orthopedic footwear |
ICD-10 codes covered if selection criteria are met: | |
| M20.10 - M20.12 | Hallux valgus (acquired) |
Cheilectomy: | |
CPT codes covered if selection criteria are met: | |
| 28289 | Hallux rigidus correction with cheilectomy, debridement and capsular release of the first metatarsophalangeal joint |
Other CPT codes related to the CPB: | |
| 11055 - 11057 | Paring or cutting of benign hyperkeratotic lesion (eg, corn or callus) |
| 73620 | Radiologic examination, foot; 2 views |
| 73630 | Radiologic examination, foot; complete, minimum of 3 views |
Other HCPCS codes related to the CPB: | |
| J0702 | Injection, betamethasone acetate 3 mg and betamethasone sodium phosphate 3 mg |
| J1020 | Injection, methylprednisolone acetate, 20 mg |
| J1030 | Injection, methylprednisolone acetate, 40 mg |
| J1040 | Injection, methylprednisolone acetate, 80 mg |
| J1094 | Injection, dexamethasone acetate, 1 mg |
| J1100 | Injection, dexamethasone sodium phosphate, 1 mg |
| J1700 | Injection, hydrocortisone acetate, up to 25 mg |
| J1710 | Injection, hydrocortisone sodium phosphate, up to 50 mg |
| J1720 | Injection, hydrocortisone sodium succinate, up to 100 mg |
| J1741 | Injection, ibuprofen, 100 mg |
| J1885 | Injection, ketorolac tromethamine, per 15 mg |
| J2920 | Injection, methylprednisolone sodium succinate, up to 40 mg |
| J3300 | Injection, triamcinolone acetonide, preservative free, 1 mg |
| J3301 | Injection, triamcinolone acetonide, not otherwise specified, 10 mg |
| J3302 | Injection, triamcinolone diacetate, per 5 mg |
| J7312 | Injection, dexamethasone, intravitreal implant, 0.1 mg |
| L3000 - L3100 | Foot inserts and arch supports |
| L3201 - L3265 | Orthopedic footwear |
ICD-10 codes covered if selection criteria are met: | |
| M20.20 - M20.22 | Hallux rigidus |
| M25.774 - M25.776 | Osteophyte, ankle and foot [painful bony spurs] |
Arthrodesis: | |
CPT codes covered if selection criteria are met: | |
| 28750 | Arthrodesis, great toe; metatarsophalangeal joint |
Other CPT codes related to the CPB: | |
| 11055 - 11057 | Paring or cutting of benign hyperkeratotic lesion (eg, corn or callus) |
| 73620 | Radiologic examination, foot; 2 views |
| 73630 | Radiologic examination, foot; complete, minimum of 3 views |
Other HCPCS codes related to the CPB: | |
| J0702 | Injection, betamethasone acetate 3 mg and betamethasone sodium phosphate 3 mg |
| J1020 | Injection, methylprednisolone acetate, 20 mg |
| J1030 | Injection, methylprednisolone acetate, 40 mg |
| J1040 | Injection, methylprednisolone acetate, 80 mg |
| J1094 | Injection, dexamethasone acetate, 1 mg |
| J1100 | Injection, dexamethasone sodium phosphate, 1 mg |
| J1700 | Injection, hydrocortisone acetate, up to 25 mg |
| J1710 | Injection, hydrocortisone sodium phosphate, up to 50 mg |
| J1720 | Injection, hydrocortisone sodium succinate, up to 100 mg |
| J1741 | Injection, ibuprofen, 100 mg |
| J1885 | Injection, ketorolac tromethamine, per 15 mg |
| J2920 | Injection, methylprednisolone sodium succinate, up to 40 mg |
| J3300 | Injection, triamcinolone acetonide, preservative free, 1 mg |
| J3301 | Injection, triamcinolone acetonide, not otherwise specified, 10 mg |
| J3302 | Injection, triamcinolone diacetate, per 5 mg |
| J7312 | Injection, dexamethasone, intravitreal implant, 0.1 mg |
| L3000 - L3100 | Foot inserts and arch supports |
| L3201 - L3265 | Orthopedic footwear |
ICD-10 codes covered if selection criteria are met: | |
| M19.071 - M19.079 | Primary osteoarthritis ankle and foot [advanced degenerative joint disease] |
| M19.171 - M19.179 | Post-traumatic osteoarthritis, ankle and foot [advanced degenerative joint disease] |
| M20.10 - M20.12 | Hallux valgus (acquired) |
| Q72.30 - Q72.33 | Congenital absence of foot and toe(s) [absent second toe] |
| S93.121+ - S93.129+ S93.141+ - S93.149+ | Dislocation and subluxation of metatarsophalangeal (joint) [severely subluxated or dislocated MTP joints] |
| Z89.421 - Z89.429 | Acquired absence of other toe(s) [absent second toe] |
The above policy is based on the following references:
Cpt Code For Distal Soft Tissue Release Date
- Canale ST, ed. Campbell's Operative Orthopaedics. 9th ed. St Louis, MO: Mosby Inc.; 1998: 1621-1694.
- Wheeless CR III, ed. Hallux valgus and bunion surgery. Wheeless Textbook of Orthopedics. CR Wheeless; 1996. Available at: http://www.medmedia.com/oo3/151.htm. Accessed April 4, 2002.
- Ferrari J, Higgins JPT, Prior TD. Interventions for treating hallux valgus (abductovalgus) and bunions. Cochrane Database Syst Rev. 2009;(2):CD000964.
- Okuda R, Kinoshita M, Morikawa J, et al. Proximal dome-shaped osteotomy for symptomatic bunionette. Clin Orthop. 2002;(396):173-178.
- Crevoisier X, Mouhsine E, Ortolano V, et al. The scarf osteotomy for the treatment of hallux valgus deformity: A review of 84 cases. Foot Ankle Int. 2001;22(12):970-976.
- Thordarson DB, Rudicel SA, Ebramzadeh E, et al. Outcome study of hallux valgus surgery--an AOFAS multi-center study. Foot Ankle Int. 2001;22(12):956-959.
- Makwana NK. Osteotomy of the hallux proximal phalanx. Foot Ankle Clin. 2001;6(3):455-471.
- Gill LH. Distal osteotomy for bunionectomy and hallux valgus correction. Foot Ankle Clin. 2001;6(3):433-453.
- Nyska M. Principles of first metatarsal osteotomies. Foot Ankle Clin. 2001;6(3):399-408.
- Veri JP, Pirani SP, Claridge R. Crescentic proximal metatarsal osteotomy for moderate to severe hallux valgus: A mean 12.2 year follow-up study. Foot Ankle Int. 2001;22(10):817-822.
- Oliver MN. What is the best treatment for patients with symptomatic mild-to-moderate hallux valgus (bunions)? J Fam Pract. 2001;50(8):718.
- Koti M, Maffulli N. Bunionette. J Bone Joint Surg Am. 2001;83-A(7):1076-1082.
- Lombardi CM, Silhanek AD, Connolly FG, et al. First metatarsophalangeal arthrodesis for treatment of hallux rigidus: A retrospective study. J Foot Ankle Surg. 2001;40(3):137-143.
- Torkki M, Malmivaara A, Seitsalo S, et al. Surgery vs orthosis vs watchful waiting for hallux valgus: A randomized controlled trial. JAMA. 2001;16;285(19):2474-2480.
- Trnka HJ. Arthrodesis procedures for salvage of the hallux metatarsophalangeal joint. Foot Ankle Clin. 2000;5(3):673-686, ix.
- Grace DL. Sesamoid problems. Foot Ankle Clin. 2000;5(3):609-627.
- Weil LS. Scarf osteotomy for correction of hallux valgus. Historical perspective, surgical technique, and results. Foot Ankle Clin. 2000;5(3):559-580.
- Robbins JM. Recognizing, treating, and preventing common foot problems. Cleve Clin J Med. 2000;67(1):45-47, 51-52, 55-56.
- Catanzariti AR, Mendicino RW, Lee MS, et al. The modified Lapidus arthrodesis: A retrospective analysis. J Foot Ankle Surg. 1999;38(5):322-332.
- Selner AJ, King SA, Samuels DI, et al. Tricorrectional bunionectomy for hallux abducto valgus. A comprehensive outcome study. J Am Podiatr Med Assoc. 1999;89(4):174-182.
- Donley BG, Tisdel CL, Sferra JJ, et al. Diagnosing and treating hallux valgus: A conservative approach for a common problem. Cleve Clin J Med. 1997;64(9):469-474.
- Donley BG. Acquired hallux varus. Foot Ankle Int. 1997;18(9):586-592.
- Brown C, Cullen N, Ferris L. Bunionette. eMedicine Journal. 2002;3(1). Available at: http://www.emedicine.com/orthoped/topic468.htm. Accessed April 4, 2002.
- Karasick D. Preoperative assessment of symptomatic bunionette deformity: Radiologic findings. AJR Am J Roentgenol. 1995;164(1):147-149.
- Moran MM, Claridge RJ. Chevron osteotomy for bunionette. Foot Ankle Int. 1994;15(12):684-688.
- Lau JT, Daniels TR. Outcomes following cheilectomy and interpositional arthroplasty in hallux rigidus. Foot Ankle Int. 2001;22(6):462-470.
- Mann RA. Intermediate to long term follow-up of medial approach dorsal cheilectomy for hallux rigidus. Foot Ankle Int. 2000;21(2):156.
- Nawoczenski DA. Nonoperative and operative intervention for hallux rigidus. J Orthop Sports Phys Ther. 1999;29(12):727-735.
- Mulier T, Steenwerckx A, Thienpont E, et al. Results after cheilectomy in athletes with hallux rigidus. Foot Ankle Int. 1999;20(4):232-237.
- Easley ME, Davis WH, Anderson RB. Intermediate to long-term follow-up of medial-approach dorsal cheilectomy for hallux rigidus. Foot Ankle Int. 1999;20(3):147-152.
- Mackay DC, Blyth M, Rymaszewski LA. The role of cheilectomy in the treatment of hallux rigidus. J Foot Ankle Surg. 1997;36(5):337-340.
- Stienstra JJ, Lee JA, Nakadate DT. Large displacement distal chevron osteotomy for the correction of hallux valgus deformity. J Foot Ankle Surg. 2002;41(4):213-220.
- Selner AJ, Selner MD, Cyr RP, Noiwangmuang W. Revisional hallux abducto valgus surgery using tricorrectional bunionectomy. J Am Podiatr Med Assoc. 2004;94(4):341-346.
- Radl R, Leithner A, Koehler W, et al. The modified distal horizontal metatarsal osteotomy for correction of bunionette deformity. Foot Ankle Int. 2005;26(6):454-457.
- Keiserman LS, Sammarco VJ, Sammarco GJ. Surgical treatment of the hallux rigidus. Foot Ankle Clin. 2005;10(1):75-96.
- Vienne P, Oesselmann M, Espinosa N, et al. Modified Coughlin procedure for surgical treatment of symptomatic tailor's bunion: A prospective followup study of 33 consecutive operations. Foot Ankle Int. 2006;27(8):573-580.
- Cohen BE, Nicholson CW. Bunionette deformity. J Am Acad Orthop Surg. 2007;15(5):300-307.
- Ferrari J. Bunions. In: BMJ Clinical Evidence. London, UK: BMJ Publishing Group; May 2008.
- Weitzel S, Trnka HJ, Petroutsas J. Transverse medial slide osteotomy for bunionette deformity: Long-term results. Foot Ankle Int. 2007;28(7):794-798.
- Legenstein R, Bonomo J, Huber W, Boesch P. Correction of tailor's bunion with the Boesch technique: A retrospective study. Foot Ankle Int. 2007;28(7):799-803.
- Giannini S, Faldini C, Vannini F, et al. The minimally invasive osteotomy 'S.E.R.I.' (simple, effective, rapid, inexpensive) for correction of bunionette deformity. Foot Ankle Int. 2008;29(3):282-286.
- Lee KB, Seo CY, Hur CI, et al. Outcome of proximal chevron osteotomy for hallux valgus with and without transverse Kirschner wire fixation. Foot Ankle Int. 2008;29(11):1101-1106.
- Lee KB, Hur CI, Chung JY, Jung ST. Outcome of unilateral versus simultaneous correction for hallux valgus. Foot Ankle Int. 2009;30(2):120-123.
- Saxena A, Nguyen A, Nelsen E. Lapidus bunionectomy: Early evaluation of crossed lag screws versus locking plate with plantar lag screw. J Foot Ankle Surg. 2009;48(2):170-179.
- Dermon A, Tilkeridis C, Lyras D, et al. Long-term results of Mitchell's procedure for hallux valgus deformity: A 5- to 20-year followup in 204 cases. Foot Ankle Int. 2009;30(1):16-20.
- Alcelik I, Alnaib M, Pollock R, et al. Bioabsorbable fixation for Mitchell's bunionectomy osteotomy. J Foot Ankle Surg. 2009;48(1):9-14.
- Guclu B, Kaya A, Akan B, et al. Stabilization of chevron bunionectomy with a capsuloperiosteal flap. Foot Ankle Int. 2011;32(4):414-418.
- Masquijo JJ, Willis BR, Kontio K, Dobbs MB. Symptomatic bunionette deformity in adolescents: Surgical treatment with metatarsal sliding osteotomy. J Pediatr Orthop. 2010;30(8):904-909.
- Waizy H, Olender G, Mansouri F, et al. Minimally invasive osteotomy for symptomatic bunionette deformity is not advisable for severe deformities: A critical retrospective analysis of the results. Foot Ankle Spec. 2012;5(2):91-96.
- Roukis TS, Meusnier T, Augoyard M. Arthrodesis of the first metatarsal-phalangeal joint with flexible, ridged titanium intramedullary nails alone or supplemented with static staples and immediate weight bearing: A consecutive series of 148 procedures. Foot Ankle Spec. 2012;5(1):12-16.
- Guha AR, Mukhopadhyay S, Thomas RH. 'Reverse' scarf osteotomy for bunionette correction: Initial results of a new surgical technique. Foot Ankle Surg. 2012;18(1):50-54.
- Kalender AM, Uslu M, Bakan B, et al. Mitchell's osteotomy with mini-plate and screw fixation for hallux valgus. Foot Ankle Int. 2013;34(2):238-243.
- Ferrari J. Hallux valgus deformity (bunion). UpToDate [serial online]. Waltham, MA: UpToDate; reviewed May 2013.
- Park YB, Lee KB, Kim SK, et al. Comparison of distal soft-tissue procedures combined with a distal chevron osteotomy for moderate to severe hallux valgus: First web-space versus trans-articular approach. J Bone Joint Surg Am. 2013;95(21):e158.
- Chao JC, Charlick D, Tocci S, Brodsky JW. Radiographic and clinical outcomes of joint-preserving procedures for hallux valgus in rheumatoid arthritis. Foot Ankle Int. 2013;34(12):1638-1644.
- National Institute for Health and Care Excellence (NICE) Website. Surgical correction of hallux valgus using minimal access techniques. February 24, 2010.
- National Guideline Clearinghouse (NCG) Website. Work Loss Data Institute. Ankle & foot (acute & chronic). August 19, 2013.
- American College of Foot and Ankle Surgeons (ACFAS) Website. ACFAS position statement on cosmetic surgery. February 2013.
- American College of Foot and Ankle Surgeons (ACFAS) Website. Clinical Practice Guideline. Diagnosis and treatment of forefoot disorders. March/April 2009.
- American College of Foot and Ankle Surgeons (ACFAS) Website. Clinical Practice Guideline. Diagnosis and treatment of metatarsophalangeal joint disorders. May/June 2003.
- Bennett GL, Sabetta JA. Evaluation of an innovative fixation system for Chevron bunionectomy. Foot Ankle Int. 2016;37(2):205-209.
- Waizy H, Jastifer JR, Stukenborg-Colsman C, Claassen L. The reverse Ludloff osteotomy for bunionette deformity. Foot Ankle Spec. 2016;9(4):324-329.
- Feng SM, Wang AG, Ding P, et al. Modified Chevron osteotomy combined distal soft tissue reconstruction to treat high-grade bunionette deformity. Zhonghua Yi Xue Za Zhi. 2016;96(28):2234-2237.
- Cetinkaya E, Yalcinkaya M, Sokucu S, et al. Cheilectomy as a first-line surgical treatment option yields good functional results in grade III hallux rigidus. J Am Podiatr Med Assoc. 2016;106(1):22-26.
- Razik A, Sott AH. Cheilectomy for hallux rigidus. Foot Ankle Clin. 2016;21(3):451-457.
- Cullen B, Stern AL, Weinraub G. Rate of revision after cheilectomy versus decompression osteotomy in early-stage hallux rigidus. J Foot Ankle Surg. 2017;56(3):586-588.
- Braito M, Dammerer D, Schlager A, et al. Continuous wound infiltration after hallux valgus surgery. Foot Ankle Int. 2018;39(2):180-188.
- Ferrari J. Hallux valgus deformity (bunion). UpToDate Inc., Waltham, MA. Last reviewed April 2018.